Mastering Pain and Management: A Comprehensive Guide
Understanding the Basics of Pain

What Exactly is Pain?
Ever stubbed your toe and felt that immediate, unmistakable sensation? That's pain, and it's your body's way of sending a signal that something's not quite right. Pain is essentially a warning system, an alert that prompts us to take action to prevent further injury.
But it's not just about physical sensations; pain has emotional and psychological components, too. It can affect your mood, your energy levels, and even your relationships. In essence, pain is a complex experience that can be both subjective and unique to each individual.
Intensity, duration, and cause are just a few aspects that can vary widely. For instance, acute pain comes on suddenly and is usually sharp in quality. It's your body's immediate reaction to an injury. Chronic pain, on the other hand, persists over time and can be resistant to medical treatments.
- Acute Pain: Sudden and sharp
- Chronic Pain: Persistent and often resistant to treatment
Remember, understanding your pain is the first step towards managing it effectively. It's important to pay attention to what your body is telling you and seek appropriate care when needed.
Different Types of Pain Explained
Pain is a complex beast, and it comes in more flavors than your favorite ice cream shop. Understanding the different types of pain is crucial because it can help you and your healthcare provider figure out the best way to tackle it.
Acute pain is like that uninvited guest at a party—it comes on suddenly and usually has a specific cause. Think of a stubbed toe or a paper cut. It's sharp, severe, but thankfully, it's often short-lived.
Chronic pain, on the other hand, is the guest that overstays their welcome. It's persistent, hanging around for weeks, months, or even years. Conditions like arthritis or back pain are the usual culprits here.
Neuropathic pain is a real wild card. It's caused by nerve damage and can feel like a shooting, burning, or even a tingling sensation. It's the kind of pain that makes you go, 'What the heck is that?'
Lastly, let's not forget about psychogenic pain, which is linked to your emotional or psychological state. It's a reminder that our minds and bodies are more connected than we might think.
- Acute Pain: Sudden and sharp
- Chronic Pain: Persistent and lingering
- Neuropathic Pain: Shooting or burning due to nerve damage
- Psychogenic Pain: Stemming from emotional or psychological factors
Remember, pain is personal. What feels like a minor annoyance to one person can be debilitating to another. So, always take pain seriously and seek professional advice when needed.
The Pain Scale: How Pain is Measured
Ever wonder how doctors figure out how much pain you're in? It's not like they can feel it themselves, right? Well, that's where the pain scale comes in handy. It's a tool that helps translate your 'ouch' into a number they can work with.
Pain scales are subjective, but they're crucial for treatment. They range from 0, which is no pain at all, to 10, the worst pain imaginable. Think of it as the 'How bad is it really?' meter.
- 0: No pain
- 1-3: Mild pain, annoying but doesn't interfere much with your day
- 4-6: Moderate pain, starts to cramp your style
- 7-9: Severe pain, it's getting hard to focus on anything else
- 10: The worst pain possible, emergency room material
Remember, your pain is unique to you. What's a '4' to you might be a '6' to someone else. It's all about how you experience it, so always be honest with your healthcare provider.
Using the pain scale during your doctor's visit can help pinpoint the best way to manage your pain. It's not just about popping pills; it's about finding the right approach for you. So next time you're asked to rate your pain, give it some thought. It could make all the difference in your care.
Lifestyle Tweaks to Keep Pain at Bay

Dietary Changes for Pain Relief
You are what you eat, and this couldn't be truer when it comes to managing pain. Inflammatory foods can exacerbate pain, while others might actually help to reduce it. It's all about striking the right balance and knowing which foods to embrace and which to avoid.
Anti-inflammatory diets are gaining traction for good reason. They focus on whole, unprocessed foods that are rich in antioxidants and have natural pain-relieving properties. Here's a quick list of some pain-fighting superfoods:
- Omega-3 rich fish like salmon and mackerel
- Leafy greens such as spinach and kale
- Berries, especially blueberries and cherries
- Nuts and seeds, including walnuts and flaxseeds
- Turmeric and ginger, known for their anti-inflammatory effects
Remember, making dietary changes is a journey, not a sprint. Start small and gradually incorporate these foods into your meals.
While it's tempting to look for a quick fix, sustainable pain relief often comes from consistent, long-term lifestyle changes. So, give your body the nutrients it needs to fight back against pain, and you might just find yourself feeling better than you have in years.
Exercise: Finding the Balance Between Rest and Movement
Finding the sweet spot between staying active and getting enough rest can be a game-changer when it comes to pain management. Exercise isn't just about pushing your limits; it's about listening to your body and understanding its needs. Too much rest can lead to stiffness and exacerbate pain, while too much movement can cause overexertion and injury.
Balance is key, and it's important to tailor your activity level to your personal pain threshold and physical capabilities. Here's a quick rundown of how to strike that balance:
- Start with low-impact activities like walking or swimming.
- Gradually increase intensity, but never to the point of pain.
- Incorporate rest days to allow your body to recover.
- Listen to your body: if it hurts, take a step back.
Remember, the goal is to maintain mobility without triggering more pain. It's not about running marathons or lifting heavy weights; it's about finding what works for you and sticking with it.
The Role of Sleep in Pain Management
It's no secret that a good night's sleep can make everything feel better, but when it comes to pain, sleep plays a crucial role. Poor sleep can actually amplify pain sensitivity, making you more susceptible to aches the next day. Conversely, quality sleep can enhance your pain threshold, giving you a stronger defense against the daily wear and tear on your body.
Sleep isn't just a time-out from daily life; it's an active period where the body repairs and rejuvenates. This includes easing inflammation, which is often a companion to pain.
To optimize your sleep for pain management, consider these tips:
- Establish a regular sleep schedule to regulate your body's clock.
- Create a restful environment, free from noise and light disturbances.
- Avoid caffeine and heavy meals before bedtime.
- Engage in relaxing activities, such as reading or taking a warm bath, to signal your body it's time to wind down.
Navigating Pain Relief Options

Over-the-Counter Solutions: What Works?
When it comes to managing pain without a prescription, there's a whole aisle at the pharmacy dedicated to over-the-counter (OTC) options. But which ones actually do the trick? Ibuprofen and acetaminophen are the heavy hitters in the world of OTC pain relief, each with its own mechanism for dialing down discomfort.
Acetaminophen is your go-to for reducing fever and relieving pain, but it's not an anti-inflammatory. It's perfect for the headaches and minor aches, just be sure to stick to the recommended dosage to keep your liver happy. On the flip side, ibuprofen not only tackles pain but also inflammation, making it a solid choice for things like sprains and dental pain.
- Aspirin, while an older remedy, still has its place, especially for heart health benefits.
- Naproxen is another anti-inflammatory that offers longer-lasting relief, ideal for those with chronic conditions.
Remember, OTC doesn't mean risk-free. Always read labels and consider any potential interactions with other medications you're taking.
While these options can be effective, they're part of a bigger pain management picture. Lifestyle changes and alternative therapies can complement these OTC warriors, giving you a well-rounded arsenal against pain.
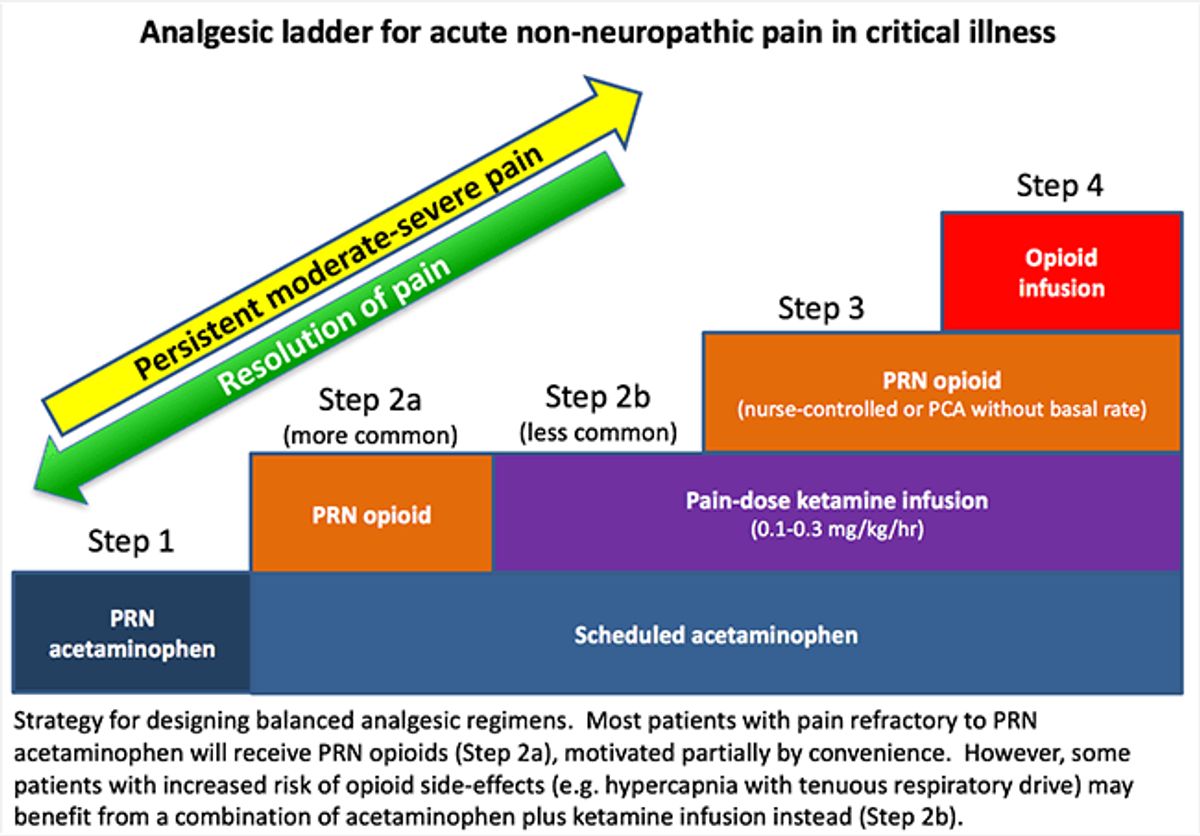
Prescription Painkillers: Risks and Benefits
Navigating the world of prescription painkillers can be like walking a tightrope. On one hand, they offer significant relief when you're in the throes of pain, but on the other, they come with a suitcase of risks that can't be ignored. The key is finding a balance that works for your body and your pain management plan.
Addiction and dependency are the big, scary words often associated with prescription meds, especially opioids. But let's not forget the potential side effects like nausea, dizziness, and constipation that can also throw a wrench in your day-to-day life.
It's crucial to have an open dialogue with your healthcare provider about the risks and benefits of prescription painkillers. They should tailor your treatment plan to minimize risks while maximizing pain relief.
Here's a quick rundown of some common prescription painkillers and their potential side effects:
- Opioids: Powerful pain relief but high risk of addiction and overdose.
- NSAIDs: Less risk of addiction but can cause stomach issues and increased risk of heart problems.
- Anticonvulsants: Used for nerve pain with fewer addiction risks but can cause drowsiness and dizziness.
- Antidepressants: Can help with chronic pain but may lead to weight gain or sexual dysfunction.
Alternative Therapies: Acupuncture, Massage, and More
When it comes to managing pain without reaching for the medicine cabinet, alternative therapies offer a world of benefits. Acupuncture, for instance, is an ancient practice that involves inserting thin needles into specific points on the body to relieve pain and improve overall wellness. It's not just about the needles, though; it's about restoring balance to your body's energy flow.
Massage therapy is another go-to for many seeking relief from muscle tension and stress-related pain. It's more than just a treat for your body; it's a holistic approach to healing that can also soothe the mind. Here's a quick rundown of some popular alternative therapies:
- Acupuncture: Balances energy flow to reduce pain
- Massage: Relieves muscle tension and promotes relaxation
- Chiropractic care: Adjusts the spine and joints to alleviate discomfort
- Aromatherapy: Uses essential oils for both physical and psychological benefits
- Yoga: Combines physical postures, breathing exercises, and meditation to enhance well-being
Remember, the effectiveness of these therapies can vary from person to person. It's important to find what works best for you and to consult with a healthcare professional before starting any new treatment regimen.
While these therapies are generally considered safe, it's crucial to seek out qualified practitioners. The right professional can make all the difference in your experience and the results you achieve. So, don't be shy to ask around, read reviews, and get recommendations to find your perfect match for pain relief.
The Mind-Body Connection in Pain Management

Meditation and Mindfulness Techniques
Tapping into the power of your mind can be a game-changer when it comes to pain management. Meditation and mindfulness are not just buzzwords; they're practical tools that can help you reduce stress and, in turn, alleviate pain. By focusing on the present moment and becoming more aware of your body and thoughts, you can actually change the way your brain perceives pain.
Consistency is key when it comes to meditation. Starting with just a few minutes each day can make a significant difference. Here's a simple way to get started:
- Find a quiet space where you won't be disturbed.
- Sit or lie down in a comfortable position.
- Close your eyes and take deep, slow breaths.
- Focus on your breath or a mantra and let go of distracting thoughts.
- Gradually increase the time you spend meditating as it becomes a habit.
Remember, it's not about achieving a state of total emptiness or having a perfect session every time. It's about the journey and the small victories along the way.
Mindfulness can be incorporated into your daily activities too. Paying attention to the sensations of simple tasks like washing dishes or walking can turn them into a form of meditation. This practice can help you stay grounded and prevent pain from taking over your life.
The Power of Positive Thinking
Harnessing the power of positive thinking can be a game-changer when it comes to pain management. It's not about ignoring the pain or living in denial; it's about shifting your focus and attitude towards a more constructive and hopeful outlook. Positive thinking can influence the body's perception of pain, potentially reducing the intensity and improving your overall quality of life.
Optimism isn't just a feel-good buzzword; it's a tool that can help you cope with pain more effectively. By fostering a positive mindset, you can create a buffer against the stress and anxiety that often accompany pain, which can actually exacerbate the sensation of discomfort.
- Recognize negative self-talk and challenge it
- Visualize positive outcomes and pain-free moments
- Practice gratitude for the good in your life, even amidst pain
Embracing positivity doesn't mean the pain will vanish, but it can mean the difference between feeling overwhelmed and feeling in control.
Remember, the journey to managing pain is as much about nurturing the mind as it is about treating the body. Incorporating positive thinking into your pain management strategy can lead to a more resilient and joyful life, even in the face of persistent pain.
Biofeedback and Other Mind-Body Therapies
Biofeedback is a technique that teaches you to control bodily processes that are typically involuntary, like heart rate or muscle tension. By using sensors that provide information about your body, this therapy can help you tune in to your body's signals. It's like becoming the conductor of your own body's orchestra, learning to harmonize functions that can influence pain perception.
- Meditation can help you focus and redirect your thoughts, which may reduce the sensation of pain.
- Yoga combines physical postures, breathing exercises, and meditation to enhance mind-body connection.
- Tai Chi, a form of martial arts, emphasizes gentle movements and can improve pain management.
Remember, the goal of mind-body therapies is not just to treat pain, but to empower you to take control of your health and well-being. These practices encourage a proactive approach to managing pain, where you're an active participant rather than a passive recipient of care.
When Pain Persists: Dealing with Chronic Pain

Understanding Chronic Pain Syndromes
Chronic pain isn't just a nagging inconvenience; it's a complex beast that can dominate your life. Unlike acute pain, which is your body's way of telling you something's wrong, chronic pain often sticks around long after an injury has healed. It's like a faulty alarm that keeps ringing even when there's no fire.
Chronic pain syndromes are varied and can include conditions like fibromyalgia, chronic fatigue syndrome, and neuropathic pain. Each of these has its own set of symptoms and challenges, but they all share one thing: the pain is persistent and often resists typical treatments.
Management of chronic pain is a journey, not a sprint. It's about finding the right combination of treatments and strategies that work for you. Here's a quick rundown of some approaches:
- Medication management
- Physical therapy
- Psychological support
- Lifestyle adjustments
Remember, managing chronic pain is about more than just dulling the discomfort. It's about improving your quality of life and finding ways to do the things you love, despite the pain.
Building a Support System
When dealing with chronic pain, the importance of a strong support system can't be overstated. Having people who understand and can provide emotional and practical support is crucial. It's not just about having someone to talk to; it's about creating a network that can help you navigate the complexities of chronic pain.
Support groups, whether online or in-person, offer a space to share experiences and coping strategies. Here's a quick list of what a good support system can offer:
- Empathy and understanding
- Shared experiences and advice
- Assistance with daily tasks
- Advocacy and help with navigating healthcare
Remember, it's okay to ask for help. Building a support system is a proactive step in managing chronic pain.
Don't underestimate the power of connection. Reaching out to friends, family, or support groups can make a significant difference in your pain management journey.
Advanced Treatments for Chronic Pain
When the usual pain management strategies don't cut it, it's time to talk about the big guns in pain relief. Advanced treatments for chronic pain are like the special ops of pain management—highly specialized and tailored to your unique situation. These treatments often involve cutting-edge technology or innovative approaches that go beyond pills and physical therapy.
Neuromodulation techniques, for example, are gaining traction. They work by altering nerve activity directly to reduce pain signals. Think spinal cord stimulators or deep brain stimulation—yeah, it sounds like sci-fi, but it's real, and it's here.
- Nerve Blocks: Injections that numb specific nerves.
- Radiofrequency Ablation: Using heat to reduce nerve sensitivity.
- Intrathecal Pumps: Delivering medication straight to the spinal fluid.
Remember, these treatments aren't first-line options. They're typically considered when other therapies haven't provided enough relief, or when pain is particularly severe and persistent.
It's crucial to have a thorough discussion with your healthcare provider about the potential risks and benefits of these advanced options. They're not for everyone, but for some, they can be a game-changer in managing chronic pain.

