Finding Relief: A Comprehensive Guide to Pain Treatments
Understanding Pain: More Than Just a Feeling

The Science of Suffering: What Happens in Your Body
Ever wonder what's really going on inside your body when you feel pain? It's not just a simple signal of 'ouch'—it's a complex biological symphony. When you get injured, your body's alarm system kicks into high gear. Nerve endings, known as nociceptors, pick up on the damage and shoot a message up to your brain, telling it to react.
- Nociceptors detect harmful stimuli
- The signal travels through the spinal cord
- The brain interprets the signal and perceives pain
Pain is your body's way of telling you something's wrong. It's a protective mechanism designed to get your attention.
But it's not just about the physical sensation. Your emotional state, past experiences, and even your expectations can shape how you feel pain. That's why two people with the same injury can have wildly different pain experiences. It's a reminder that pain is personal, and what works for one person's relief might not work for another.
Types of Pain: Acute vs Chronic
Ever stubbed your toe and felt that immediate, sharp twinge? That's acute pain, folks – it jumps out at you, yells 'hello,' and then usually fades away as the injury heals. Chronic pain, on the other hand, is like that uninvited guest who just won't leave. It sticks around for weeks, months, or even years, and it's often due to conditions like arthritis or back problems.
- Acute Pain: Sudden onset, usually a clear cause, short-term
- Chronic Pain: Persistent, can be due to an ongoing issue, long-term
Remember, chronic pain isn't just a prolonged version of acute pain; it's a different beast altogether. It can mess with your mood, sleep, and overall quality of life. So, it's super important to understand which type you're dealing with to manage it effectively.
Pain Perception: Why It's Different for Everyone
Ever wonder why a paper cut feels like a mere annoyance to some but a major ordeal to others? Pain perception is as unique as a fingerprint, varying widely from person to person. This variability can be attributed to a number of factors, including genetic makeup, stress levels, and even past experiences.
Genetics play a pivotal role in how we experience pain. For instance, some people have a higher natural tolerance and may not feel the need for pain relief as quickly as others. On the flip side, there are those who are more sensitive and may require intervention for the same level of discomfort.
- Stress and emotional state can amplify pain sensations.
- Past injuries or traumas can alter our pain threshold.
- Cultural and social backgrounds can shape how we express and manage pain.
It's crucial to remember that pain is subjective. What might be a minor nuisance to one person could be debilitating to another. Healthcare providers should always take a patient's personal pain report seriously, tailoring treatment to their specific needs.
Medication Matters: Finding What Works for You

Over-the-Counter Options: What to Consider
When you're facing mild to moderate pain, over-the-counter (OTC) medications can be a real lifesaver. But before you reach for that bottle, it's important to understand what you're taking and how it affects your body. Always read the label and follow the dosage instructions to avoid any adverse effects.
Aspirin, ibuprofen, and acetaminophen are the most common OTC pain relievers. Each has its own set of benefits and potential risks:
- Aspirin: Reduces inflammation and can help with pain, but not recommended for everyone, especially those with certain medical conditions.
- Ibuprofen: Good for inflammation and pain, but can cause stomach upset in some people.
- Acetaminophen: Effective for pain relief, but be cautious with the dosage to avoid liver damage.
Remember, OTC medications can interact with other drugs and dietary supplements, so it's crucial to talk to your pharmacist or doctor if you're taking multiple treatments.
While OTC options are convenient, they're not a one-size-fits-all solution. If your pain persists or worsens, don't hesitate to consult a healthcare professional for further advice.
Prescription Painkillers: Use with Caution
When it comes to prescription painkillers, it's crucial to strike a balance between relief and risk. These powerful meds, like opioids, can be game-changers for those with severe pain, but they come with a hefty price tag of potential addiction and side effects. Always follow your doctor's guidance and never stray from the prescribed dosage.
Addiction isn't the only concern. Side effects can range from drowsiness to more serious issues like respiratory depression. Here's a quick rundown of what to watch out for:
- Drowsiness or sedation
- Nausea or vomiting
- Constipation
- Itching or rash
- Respiratory depression
Remember, your health history and current medications can significantly influence how you react to painkillers. It's a conversation worth having with your healthcare provider.
Lastly, keep an open dialogue with your doctor about how you're feeling. If something's off, or if the pain persists, there might be other treatments to explore. Prescription painkillers are a tool, not a cure-all, and should be used as part of a broader pain management plan.
Alternative Remedies: Herbal and Beyond
When it comes to managing pain, sometimes the best treasures are found in nature's own medicine cabinet. Herbal remedies have been used for centuries to alleviate discomfort, and modern science is beginning to catch up with traditional knowledge. From the anti-inflammatory properties of turmeric to the soothing effects of chamomile, there's a plethora of herbs that can offer relief.
Remember, natural doesn't always mean harmless. It's crucial to consult with a healthcare provider before starting any herbal regimen, especially if you're taking other medications.
Here's a quick list of some popular herbal remedies and their common uses:
- Turmeric: Often used to reduce inflammation.
- Ginger: Can help with nausea and muscle pain.
- Willow Bark: Known as 'nature's aspirin' for its pain-relieving qualities.
- Peppermint: May soothe digestive issues and headaches.
While exploring alternative remedies, keep an open mind but also maintain a healthy dose of skepticism. Not all remedies will work for everyone, and some may interact with other treatments. Personal research and professional guidance are your best allies in finding what works for you.
Lifestyle Tweaks: Natural Ways to Ease the Ache

Diet and Nutrition: Foods That Fight Pain
You are what you eat, and that couldn't be truer when it comes to managing pain. Certain foods have anti-inflammatory properties that can help reduce chronic pain or flare-ups. For instance, omega-3 fatty acids found in fish like salmon and mackerel can be powerful allies in your fight against discomfort.
Incorporating antioxidants into your diet is also key. Foods rich in these compounds, such as berries, leafy greens, and nuts, can help protect your body's cells from damage and reduce inflammation. Here's a quick list of pain-fighting foods to add to your grocery cart:
- Ginger
- Turmeric
- Olive oil
- Cherries
- Pumpkin seeds
Remember, no single food is a miracle cure, but a balanced diet full of these pain-relieving foods can make a significant difference in how you feel.
It's not just about what you eat, but also what you avoid. Processed foods, sugary snacks, and high-sodium items can exacerbate pain by increasing inflammation. Strive for a diet that's as natural and unprocessed as possible to give your body the best chance at healing.
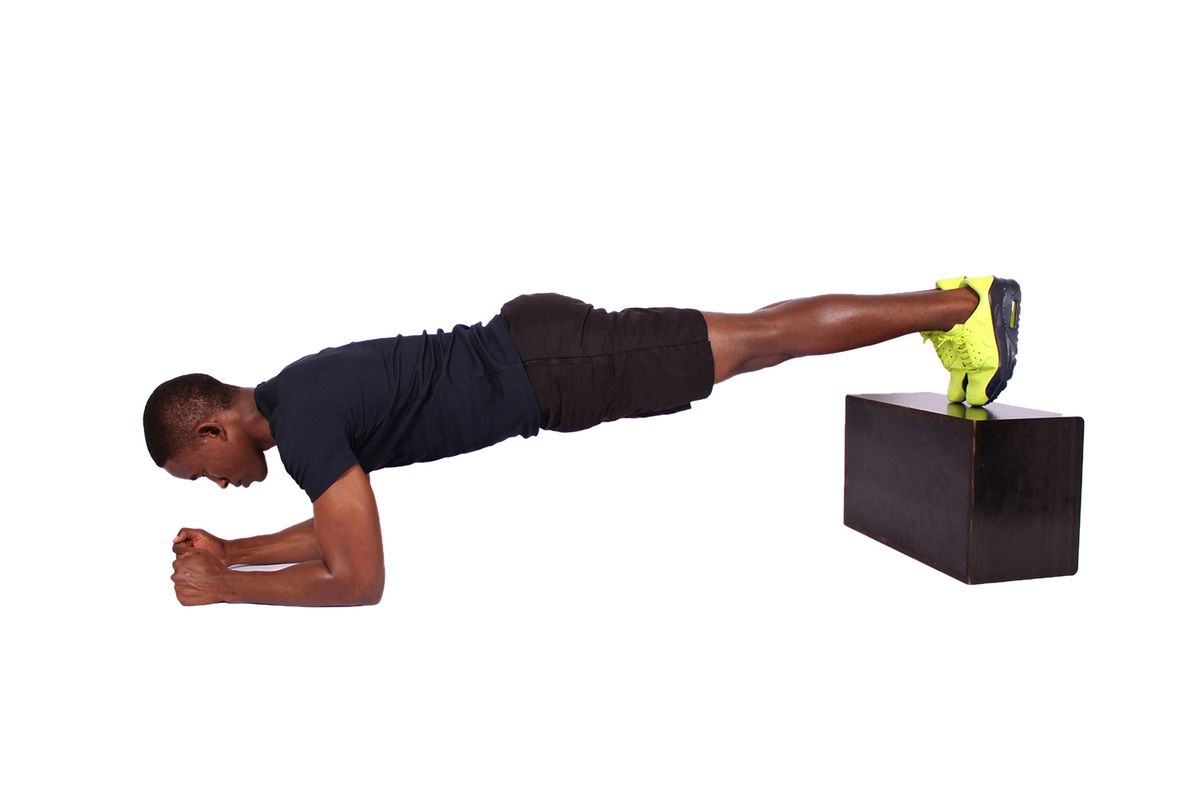
Exercise: Moving to Manage Discomfort
It's no secret that staying active can be a game-changer when it comes to pain management. Regular exercise not only boosts your overall health but can also reduce the intensity and frequency of pain episodes. It's about finding the right balance and not overdoing it, as too much exercise can actually exacerbate pain.
Movement is medicine for the body, and incorporating a variety of activities can help keep things interesting and effective. Here's a quick rundown of exercises that can help ease the ache:
- Low-impact activities: such as swimming or cycling, which are gentle on the joints.
- Strength training: to build muscle support around painful areas.
- Flexibility exercises: like yoga or stretching, to improve range of motion.
- Aerobic exercises: walking or jogging can increase endorphin levels, the body's natural painkillers.
Remember, it's crucial to listen to your body and adjust your exercise routine accordingly. If something hurts, take a step back and try a different activity or approach.
Before starting any new exercise regimen, it's wise to consult with a healthcare professional, especially if you're dealing with chronic pain. They can help tailor a program that's right for you and ensure you're moving in a safe and beneficial way.
Mind-Body Techniques: Meditation, Yoga, and More
Tapping into the power of your mind can have surprising effects on your experience of pain. Mind-body techniques like meditation and yoga are not just trendy; they're backed by science to help reduce stress and pain perception. By focusing on breathing and mindfulness, you can often find a sense of calm that helps to ease the ache.
Yoga, for instance, combines physical postures with breathing exercises and meditation, promoting both physical and mental wellness. It's not about twisting yourself into a pretzel; it's about finding balance and harmony within your body.
- Meditation: A practice of focused attention to achieve mental clarity.
- Yoga: A holistic approach combining postures, breathing, and meditation.
- Tai Chi: Gentle movements to promote serenity and healing.
Remember, the goal isn't to become a master overnight. It's about incorporating small practices into your daily routine that can lead to big changes in how you feel.
While these practices may not eliminate pain completely, they can be an essential part of a comprehensive pain management plan. It's all about finding what resonates with you and integrating it into your life for the long haul.
Professional Help: When to Seek a Specialist
Physical Therapy: Rebuilding Strength and Mobility
Physical therapy is a cornerstone in the management of many pain conditions, especially when it comes to musculoskeletal issues. It's not just about exercises; it's about retraining your body to move in ways that alleviate pain and improve function. A physical therapist can tailor a program specifically to your needs, which may evolve as you progress.
Physical therapy often includes a mix of techniques, such as:
- Manual therapy to manipulate muscles and joints
- Therapeutic exercises to strengthen weak areas
- Pain relief methods like heat or cold therapy
- Education on posture and body mechanics to prevent future injuries
Remember, consistency is key. The benefits of physical therapy are most pronounced when you stick with the program and apply what you learn to your daily life.
Finding the right physical therapist is crucial. Look for someone who listens to your concerns and has experience with your particular type of pain. They should be a partner in your journey to recovery, providing not just treatment but also support and motivation.
Pain Clinics: Comprehensive Care Teams
When you're at your wit's end with pain, a pain clinic might just be your new best friend. These clinics offer a holistic approach, bringing together specialists from various fields to tackle your pain from every angle. The goal is to create a personalized treatment plan that addresses not just the symptoms, but the root causes of your pain.
- Pain management specialists
- Physical therapists
- Occupational therapists
- Psychologists
- Nurses
Each member of the team has a unique role, ensuring that all aspects of your pain are considered. For instance, while a pain management specialist may focus on medication or injections, a physical therapist will help you strengthen your body and reduce the risk of further injury.
Remember, the journey to managing pain is a marathon, not a sprint. It takes time, patience, and a dedicated team to make real progress.
Surgical Options: Last Resort or Necessary Step?
Deciding to undergo surgery for pain relief is a significant decision that should not be taken lightly. It's crucial to weigh the potential benefits against the risks and recovery time. Surgery might be considered a last resort when other treatments have failed, or it could be a necessary step for certain conditions that don't respond to less invasive methods.
Recovery from surgery can vary greatly depending on the procedure and the individual. It's important to have a clear understanding of the post-operative care and the rehabilitation process. Here's a quick rundown of what to expect:
- Pre-surgical assessments to determine suitability and risks
- A detailed explanation of the procedure and expected outcomes
- Post-operative care, including pain management and physical therapy
Remember, the goal of surgery is to improve your quality of life. It's a journey that requires patience, commitment, and a supportive medical team.
Always consult with a healthcare professional to discuss the specifics of your situation and to understand if surgery is the right option for you. The decision should be a collaborative one, made with your long-term health and well-being in mind.
Navigating the Emotional Toll of Chronic Pain

Coping Strategies: Keeping Your Spirits Up
Living with chronic pain can be a daily battle, not just physically but emotionally too. Finding ways to maintain a positive outlook is crucial for your overall well-being. One effective strategy is to set small, achievable goals each day. This can help you focus on what you can do, rather than what you can't.
Journaling your thoughts and feelings can also be a therapeutic outlet. It allows you to express yourself and reflect on your experiences in a constructive way. Here's a simple list to get started with journaling:
- Write down three things you're grateful for every morning.
- Note any new pain patterns or triggers.
- End your day by jotting down a positive experience, no matter how small.
Remember, it's okay to have bad days. Accepting your emotions as part of the healing process can lead to greater resilience.
Connecting with others who understand what you're going through can make a world of difference. Consider joining a support group or an online community. Sharing your journey and hearing others' stories can provide comfort and new coping strategies.
Support Networks: Finding Community
Finding a community of individuals who understand what you're going through can be a game-changer in managing chronic pain. Support groups offer a space to share experiences, tips, and encouragement. They can be found in various places:
- Local community centers
- Hospitals and clinics
- Online forums and social media groups
Engaging with a support network can help alleviate the sense of isolation that often accompanies chronic pain. It's important to remember that while each person's pain is unique, you're not alone in this journey.
By connecting with others, you can discover new coping strategies and feel more empowered to tackle the daily challenges of living with pain.
Remember, the goal of joining a support network is not just to receive support, but also to give it. The mutual exchange of empathy and understanding can be incredibly therapeutic.
Mental Health and Pain: The Inextricable Link
It's no secret that chronic pain can take a toll on your mental health. The constant discomfort can lead to feelings of frustration, depression, and anxiety. Managing both pain and mental health is crucial for overall well-being. It's important to recognize that seeking help for mental health is as vital as treating physical pain.
Stress can exacerbate pain, creating a vicious cycle that's hard to break. Here are a few strategies to help keep your mental health in check:
- Practice relaxation techniques like deep breathing or progressive muscle relaxation.
- Set realistic goals and celebrate small victories.
- Stay connected with friends and family who understand what you're going through.
Remember, it's okay to not be okay. Acknowledging your emotional state is the first step towards healing both your mind and your body.